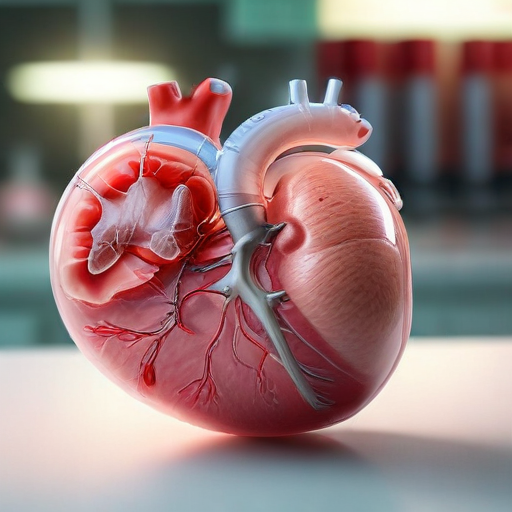
According to the World Economic Forum (WEF), there is a significant disparity between the demand for organ transplants and the availability of suitable donors. Over the past thirty years, advancements in gene editing have shown promise in addressing this gap, potentially enabling the transplantation of animal organs into humans.
Innovative technologies like CRISPR-Cas9 have allowed researchers to modify pig genes to eliminate viral genes that could pose risks to human patients. This genetic manipulation, coupled with specific drug therapies, has enabled non-human primates to survive for extended periods—some experiencing months or even years—with transplanted pig kidneys and hearts.
If xenotransplantation, which involves using animal organs for human transplants, becomes a standard therapeutic option, it could greatly enhance the quality of life for millions awaiting organ transplants. Additionally, it could significantly influence the healthcare economy, as highlighted by the WEF.
Moreover, the exploration of genomic understanding may extend beyond organ transplants, suggesting that specialized pig cells might offer therapeutic benefits for conditions such as diabetes and Parkinson’s disease. However, the practice of xenotransplantation also brings forth ethical considerations that require thorough examination.
In summary, while the prospect of using engineered animal organs presents a groundbreaking solution to the organ shortage crisis, it necessitates careful deliberation on the ethical implications involved. As scientists continue to innovate, there is hope for improved methods that not only address organ shortages but could also pave the way for advancements in treating chronic health conditions. This journey showcases the potential of science to enhance human health and well-being in the future.