A new international study indicates that COVID-19 infection can accelerate vascular aging, with the effect most evident in women. The CARTESIAN study followed 2,390 people across 16 countries from 2020 to 2022 and used carotid-femoral pulse wave velocity (PWV) as a marker of large-artery stiffness.
Key findings
– COVID-19 exposure was linked to higher PWV, signaling stiffer arteries and an older vascular age. Compared with COVID-negative controls, COVID-positive participants had higher PWV across all severity groups: hospitalized (+0.37 m/s), ICU (+0.40 m/s), and non-hospitalized (+0.41 m/s).
– The vascular aging signal was strongest among women, who showed PWV increases ranging from +0.55 to +1.09 m/s depending on COVID severity.
– The study is described by its authors as the first adequately powered analysis to quantify how COVID-19–linked vascular aging relates to disease severity and to show that sex modifies this association.
– Among women, those reporting persistent long COVID symptoms at six months tended to have higher PWV than those who recovered, suggesting PWV could reflect ongoing vascular injury or inflammation in female patients with prolonged symptoms. In men, PWV did not differ much between those with and without persistent symptoms.
What the data suggest about mechanisms
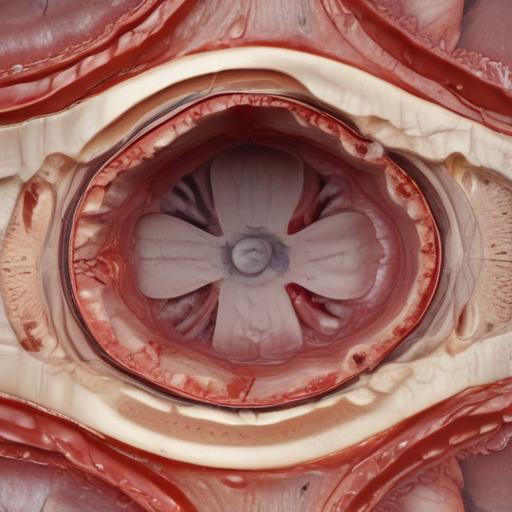
– The virus targets cells via the ACE2 receptors found on blood vessel linings, which can lead to vascular dysfunction and accelerated aging.
– Sex differences in immune response may partly explain the disparity: women mount robust immune reactions that, while protective against infection, may contribute to greater vascular damage after acute infection.
Longer-term observations and interpretation
– Over about a year, participants who recovered from COVID generally had stable or improved PWV, while uninfected controls tended to show PWV increases. The authors note that the small post-acute rise in PWV in the COVID group could reflect normal aging or possible undiagnosed reinfection.
– There remains the possibility of irreparable vascular damage in some patients, but improvements in factors tied to autonomic regulation and inflammation could help reduce PWV over time.
– The study was not designed to assess treatment effects (for example, statins) and acknowledges potential biases, including survival bias and pre-existing vascular aging before infection.
Vaccination and risk management
– Vaccination was associated with lower PWV in this real-world study, although the observational design cannot fully separate vaccination effects from other differences between vaccinated and unvaccinated groups.
– The researchers underscore that vascular aging is measurable and, where present, potentially modifiable through established interventions—locusing on blood pressure control, lipid management, healthy lifestyle changes, and cardiovascular risk reduction.
Clinical and public-health implications
– PWV could become a useful physiological marker to identify post-COVID patients at higher risk of vascular injury, especially among women with persistent symptoms.
– Clinicians may consider incorporating PWV assessments into follow-up care for patients recovering from COVID-19, particularly those with long COVID symptoms.
– The findings reinforce the broader message that reducing cardiovascular risk factors remains important for survivors of COVID-19, and that vaccination may confer vascular benefits beyond infection prevention.
Additional value and context
– The CARTESIAN study encompassed a diverse international cohort, enhancing the generalizability of its findings. Its results align with the growing recognition that sex-specific responses influence long-term sequelae of COVID-19.
– While promising, PWV should be interpreted within the study’s limitations, and ongoing research will clarify how best to integrate these measurements into routine care and whether targeted interventions can reverse COVID-related vascular aging more robustly.
Summary
– COVID-19 is associated with accelerated vascular aging, particularly in women, as shown by increased PWV across COVID-positive groups.
– Over time, PWV may stabilize or improve, suggesting potential reversibility with time and risk-factor management.
– Vaccination appears linked to lower PWV, but causality can’t be established from this observational study.
– PWV holds potential as a practical marker for monitoring vascular health in post-COVID patients and guiding preventive strategies.
Positive note
– The finding that PWV can improve or stabilize over time provides a hopeful angle: with appropriate cardiovascular risk management and lifestyle changes, some of the vascular effects of COVID-19 may be mitigated, reducing the longer-term risk of heart attack or stroke for survivors.
If you’d like, I can adapt this into a shorter summary for social media or expand it with expert quotes to accompany a feature on post-COVID cardiovascular health.